Is My Pain All in My Head?
Understanding pain, the brain, and how the nervous system affects healing
At some point we’ll all experience pain and we might question if it’s all in our head.
The short answer to that question is - no. Pain is real and it’s also complex.
But, that doesn’t mean it has to be so scary and the more we understand about pain, the less of a hold it has on us.
That’s why one of my missions as a physical therapist is to help you understand your pain so you can work with it rather than letting it run your life.
Imagine this…
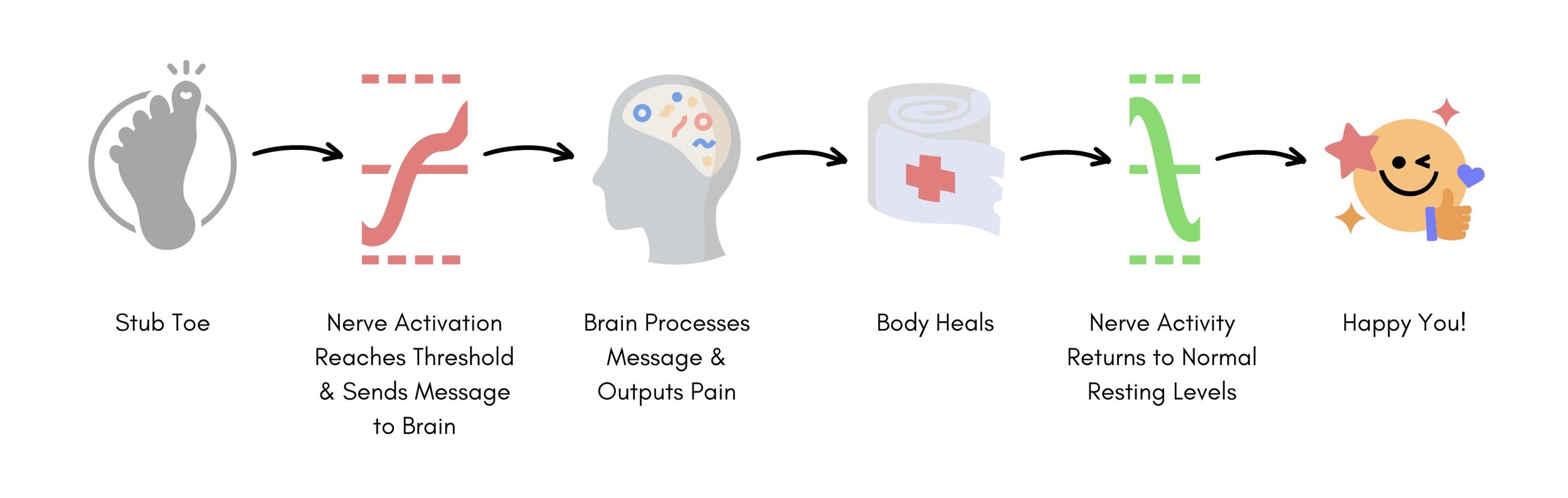
You get out of bed in the morning, groggy and definitely not awake yet, and, you stub your toe - hard - on the bed frame.
You have immediate pain (and maybe a few choice words, iykyk) and limp around for a bit. After a few minutes, the pain has mostly gone away and you carry on with your day.
What happened that resulted in pain?
All throughout our body we have sensors (nerves) that send signals to our brain through our nervous system. In fact, we have 45 miles of nerves that connect our body! That’s a pretty impressive highway system, huh?
All of our nerves have a bit of “electricity” coursing through them and even at rest they’re a little bit active.
When we have an input into our system - like stubbing our toe - the activity of the nerves increase and if that activity reaches a certain threshold the nerves send a “danger” signal to our brain.
Once that “danger” signal reaches our brain, our brain processes it to determine if there is a threat to our safety or not. If it is a threat to our safety, our brain outputs pain and we act in accordance - we limp, move our hand off the hot stove, etc.
In most cases, as our injury heals the activity in our nerves decreases and returns to normal resting levels and we no longer experience pain.
Unfortunately, there are times that this decrease in nerve activity doesn’t happen and that can lead to long standing pain.
What’s happening when your pain doesn’t go away?
Sometimes when we heal from an injury, our nerves remain sensitive and continue to fire at a higher level than they were prior to injury. In this case, it takes less input into our system to have our nerves activated and generate a danger signal.
Practically speaking, an activity that once used to feel easy - doing the dishes, going for a walk, sitting for work - now results in pain. That’s a serious bummer and can have a huge impact on our quality life and our well-being!
Some things that can impact the sensitivity of our nerves include:
Family, household, and/or relationship stress or demands
Fear - of another injury, of continued pain, of not being able to do the things you want or need to do
Financial concerns
How you’ve healed from a previous injury or how you’ve seen others heal from a similar injury
Illness, allergies, autoimmune conditions
Job issues
Nutrition and/or hydration
Poor sleep
Stress
Travel
Etc.
Decreasing the sensitivity of our nerves
It’s not all bad news, I promise!
We can have a positive influence on our pain experience, decreasing the sensitivity of our nerves and nervous system, through things like:
Mindfulness practices
Deep breathing
Sleep hygiene and improving our sleep quality
Activity pacing
Graded exposure to activity
Movement practices
Some folks also find these phrases helpful to remember:
Motion is Lotion - movement brings more blood flow and hydration to our joints and tissues and they LOVE that!
Sore but Safe - soreness does not always equate to injury. Maybe you can even remember times you’ve worked out and had soreness that felt good.
Hurt not Harm - just because there’s pain doesn’t mean there’s injury.
If you’ve been struggling to find a compassionate approach to relieving your pain, schedule a physical therapy appointment so you can get the support you need on your journey to healing.
References
Louw A. Pain Neuroscience Education. Presented: Therapeutic Neuroscience Education at Evidence In Motion; January 2020. Online.
Louw, A. Why do I hurt? A patient book about the neuroscience of pain. Minneapolis, MN: OPTP; 2013.
Louw, A. Pain Neuroscience Education: Teaching People About Pain 2nd ed. Minneapolis, MN: OPTP; 2018.
Disclaimer: this post is intended for informational purposes only and is not medical advice. If you are experiencing pain, it is always in your best interest to consult with your medical doctor and/or your physical therapist.